CASE REPORT | https://doi.org/10.5005/jp-journals-10057-0127 |
A Rare Case of “Symptomatic Bilateral Adrenal Myelolipoma”
1–4Department of Pathology, Mahatma Gandhi Medical College and Hospital, Jaipur, Rajasthan, India
Corresponding Author: Niharika Jain, Department of Pathology, Mahatma Gandhi Medical College and Hospital, Jaipur, Rajasthan, India, Phone: +91 9993252552, e-mail: niharika.oct10@yahoo.in
How to cite this article Jain N, Gautam P, Mathur A, et al. A Rare Case of “Symptomatic Bilateral Adrenal Myelolipoma”. J Mahatma Gandhi Univ Med Sci Tech 2020;5(3):100–102.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Introduction: Adrenal myelolipoma is a benign neoplasm composed of mature adipose tissue and scattered islands of hematopoietic elements. Although the true incidence of these tumors is unknown, the incidence estimated to be is quite less. These lesions are usually unilateral and asymptomatic and are very rarely found as bilateral tumors.
Aims and objectives: To present a rare case of “Symptomatic Bilateral Adrenal Myelolipoma”.
Materials and methods: A 53-year-old woman presented with complaints of pain abdomen for 6 months. Physical examination was unremarkable. Computed tomography (CT) scan of the abdomen revealed a well-defined, round lesion bilaterally with heterogeneous attenuation suggesting the possibility of myelolipoma. The patient was subjected to bilateral adrenalectomy and the bilateral adrenal masses were sent for histopathological examination.
Results: The histopathological evaluation of masses confirmed the diagnosis of bilateral adrenal myelolipoma.
Conclusion: Although mostly discovered as an “incidentaloma”, the diagnosis of adrenal myelolipoma warrants through diagnostic study. Surgical resection is the mainstay as it prevents complications, such as spontaneous rupture and hemorrhage of the mass.
Keywords: Adipose tissue, Adrenal gland, Hematopoietic, Incidentaloma, Myelolipoma.
INTRODUCTION
Myelolipoma is a rare, non-functional, benign neoplasm that predominantly occurs in the adrenal cortex. In 1905, Gierke first described the occurrence of a mass lesion in the adrenal glands composed of mature fat and mixed myeloid and erythroid cells.1 It is the second most common tumor of the adrenal cortex, the first being adenoma.2 It comes under the category of mesenchymal and stromal tumors of the adrenal gland. It is composed of mature adipocytes and normal hematopoietic tissue. Although they do not represent a hematopoietic source, they contain hematopoietic elements consisting of myeloid and erythroid precursors as well as megakaryocytes. The incidence is unknown, it is estimated to be 0.08–0.25% accounting for 2.6% of all primary adrenal tumors.2–4 Earlier it was more commonly seen in subjects during an autopsy; however, recently myelolipomas are being increasingly detected in living patients by imaging techniques. They are often seen in patients in their fifth to seventh decade of life and show female predominance. Myelolipoma is twice as common on the right side as on the left. They are usually unilateral and asymptomatic and are rarely found bilaterally.5 Around 40 bilateral cases have been reported in the literature.2
CASE DESCRIPTION
A 53-year-old woman presented to surgery OPD with complaints of pain in the abdomen for 6 months. Physical examination was unremarkable. Computed tomography (CT) scan revealed a well-defined, round lesion bilaterally with heterogeneous attenuation, size being larger at the left side. Hematological investigations including hemogram, cortisol levels, biochemical parameters, liver function tests, renal function tests, and electrolytes (Na, K, Cl) were within normal limits. The patient underwent bilateral adrenalectomy and the masses were sent for histopathological examination.
PATHOLOGICAL FINDINGS
Macroscopically, the specimen consisted of two specimens labeled as right and left adrenal gland.
The right adrenal gland measured 9 × 7 × 5 cm and the left adrenal gland measured 16 × 14 × 6 cm. The external surface of both the glands was hemorrhagic. Cut surface showed a tumor that was gray-yellow to gray-brown in color and showed hemorrhagic areas (Fig. 1).
Microscopically, normal adrenal tissue was seen at the periphery along with adipocytes with interspersed hematopoietic elements comprising of myeloid and erythroid precursors as well as megakaryocytes. Features were consistent with myelolipoma (Figs 2 to 4).
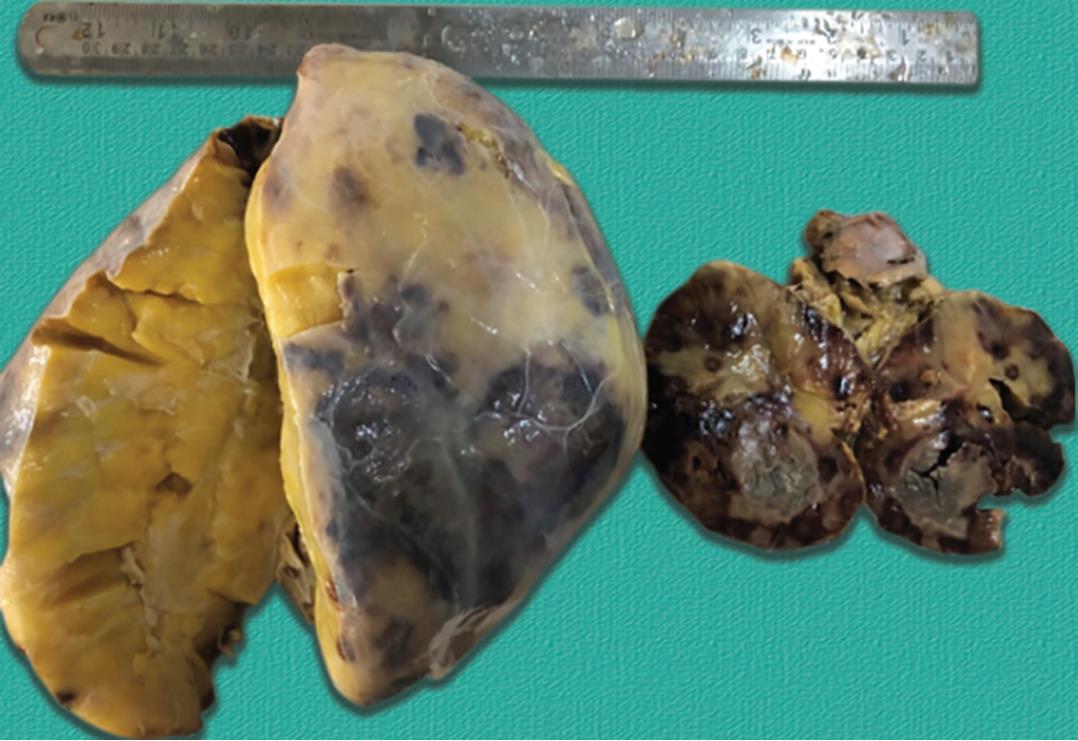
Fig. 1: Gray-yellow to gray-brown in color showed hemorrhagic areas
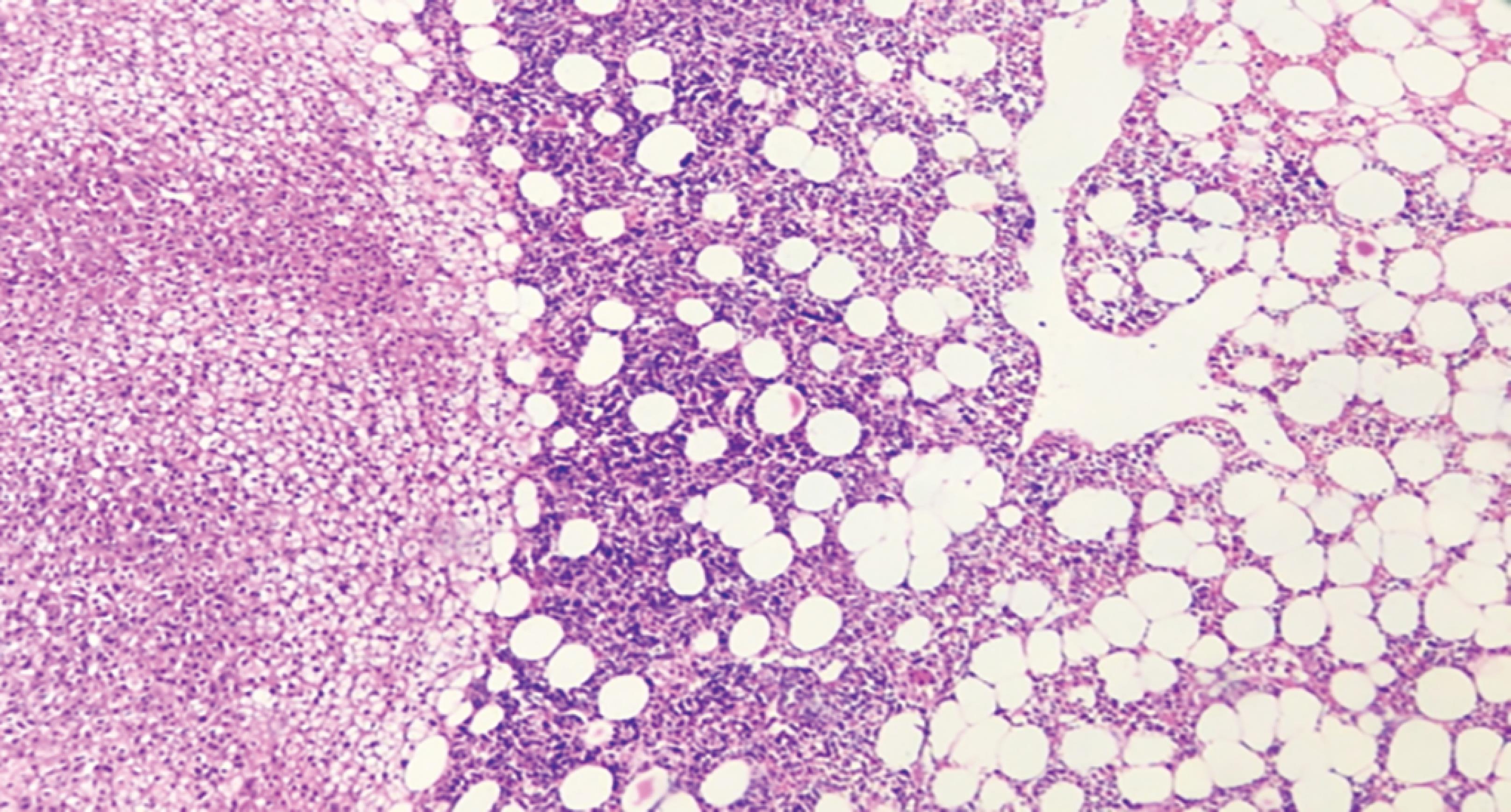
Fig. 2: Scanner view
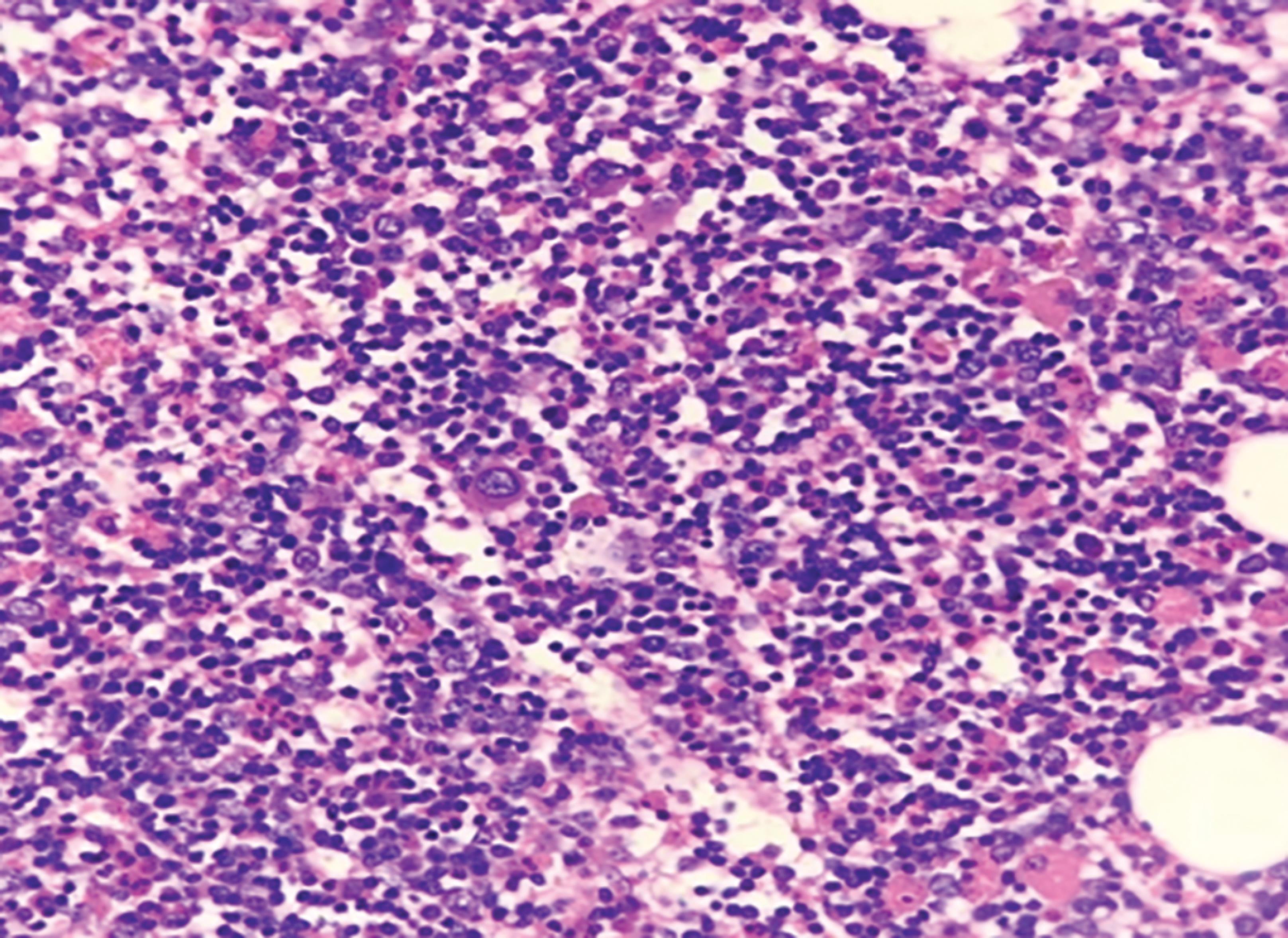
Fig. 3: Low power

Fig. 4: High power
DISCUSSION
Bilateral adrenal myelolipoma constitutes a rare entity in urological practice.
Although its pathogenesis remains unknown, the most widely accepted theory is the presence of metaplasia of reticuloendothelial cells of blood capillaries in the adrenal in response to stimuli such as stress, necrosis, or infection. However, the most widely accepted theory is adrenocortical cell metaplasia in response to stimuli, such as necrosis, inflammation, or stress.6 In 1905, Gierke described this entity1 and Dyckman and Freedman reported the first case of surgical removal.7 In 1985, deBlois and DeMay reported the first case of a myelolipoma which was based on radiographic findings.8 There are several theories for the etiology and natural history of adrenalmyelolipoma.9–11
The conditions often associated with adrenal myelolipomas include Cushing’s disease, obesity, hypertension, and diabetes which are considered as major adrenal stimuli.12 Other contemporary authors have speculated about a stressful lifestyle and an unbalanced diet as factors that may be involved in the pathogenesis of this tumor.13
Ultrasonography, CT, and magnetic resonance imaging (MRI) are all effective in diagnosing most of the adrenal myelolipoma based on the identification of fat, with CT scan considered as the most sensitive.14,15 Since the occasional of these tumors are functional, an endocrinological evaluation may not be useful. The differential diagnosis should include renal angiomyolipoma, retroperitoneal lipoma, and liposarcoma.
No malignant progression has been reported. Most cases are followed by observation. Retroperitoneal hemorrhage has been reported, and large/symptomatic tumors are managed by surgery.
CONCLUSION
Adrenal myelolipomas are rare tumors, mostly of benign nature, and clinically silent. However, their “incidental” findings should warrant careful diagnostic study so that appropriate management can be planned. Imaging modalities, such as, ultrasonography and CT, can yield the diagnosis. There is an increasing number of myelolipomas reported which necessitate the use of thorough workup including biochemical studies. Surgical resection is the mainstay as it minimizes postoperative complications and leads to a quicker recovery.
REFERENCES
1. Gierke E. Uber knochenmarksgwebe in der nebenniere. Zeiglers Beitr Path Anat 1905 (Suppl. 7):311–324.
2. Lam AKY, Chuah KL, de Pinieux G, et al. World Health Organization Classification of Tumours of Endocrine Organs.Lyon: IARC Press; 2017.
3. Olsson CA, Krane RJ, Klugo RC, et al. Adrenal myelolipoma. Surgery 1973;73:665.
4. McDonnell WV. Myelolipoma of adrenal. Arch Path 1956;61:416.
5. Lack E, Wienke J. Diagnostic Histopathology of Tumors Fletcher CDM, ed., vol. 1(4th ed.,) Elsevier Saunders; 2013.
6. Meyer A, Behrend M. Presentation and therapy of myelolipoma. Int J Urol 2005;12(no. 3):239–243. DOI: 10.1111/j.1442-2042.2005.01034.x.
7. Dyckman J, Freedman D. Myelolipoma of the adrenal with clinical features and surgical excision. J Mt Sinai Hosp 1957;24:793.
8. deBlois GG, DeMay RM. Adrenal myelolipoma diagnosis by computed-tomography-guided fine-needle aspiration. A case report. Cancer 1985;55(4):848. DOI: 10.1002/1097-0142(19850215)55:4<848::AID-CNCR2820550423>3.0.CO;2-2.
9. Vierna J, Laforga JB. Giant adrenal myelolipoma. Scand J Urol Nephrol 1994;28(no. 3):301–304. DOI: 10.3109/00365599409181284.
10. Boudreaux D, Waisman J, Skinner DG, et al. Giant adrenal myelolipoma and testicular interstitial cell tumor in a man with congenital 21-hydroxylase deficiency. Am J Surg Pathol 1979;3(2)):109–123. DOI: 10.1097/00000478-197904000-00002.
11. Han M, Burnett AL, Fishman EK, et al. The natural history and treatment of adrenal myelolipoma. J Urol 1997;157(no. 4):1213–1216. DOI: 10.1016/S0022-5347(01)64926-7.
12. Tyritzis SI, Adamakis I, Migdalis V, et al. Giant adrenal myelolipoma, a rare urological issue with increasing incidence: a case report. Cases J 2009;2(no. 9):8863. DOI: 10.4076/1757-1626-2-8863.
13. Daneshmand S, Quek ML. Adrenal myelolipoma: Diagnosis and management. J Urol 2006;3:71–74.
14. Kenney PJ, Wagner BJ, Rao P, et al. Myelolipoma: CT and pathologic features. Radiology 1998;208(no. 1):87–95. DOI: 10.1148/radiology.208.1.9646797.
15. Répássy DL, Csata S, Sterlik G, et al. Giant adrenal myelolipoma. Pathol Oncol Res 2001;7(1):72–73. DOI: 10.1007/BF03032610.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.